Appendix D
The Importance of Breastfeeding
Appendix D References
- Boron-at-Catalá, M., Montiel-Company, J. M., Bellot-Arcís, C., Almerich-Silla, J. M., & Catalá-Pizarro, M. (2017). Association between duration of breastfeeding and malocclusions in primary and mixed dentition: a systematic review and meta-analysis. Scientific Reports, 7(1):5048. https://doi.org/10.1038/s41598-017-05393-y
- Centers for Disease Control and Prevention. (2022, August 4). Frequently Asked Questions (FAQs): How long should a
mother breastfeed? Centers for Disease Control and Prevention. https://www.cdc.gov/breastfeeding/faq/index.htm#:~:text=Th
e%20American%20Academy%20of%20Pediatrics%20and%20the%20World%20Health%20Organization,years%20of%20age%20or%20longer. - Chantry, C. J., Dewey, K. G., Peerson, J. M., Wagner, E. A., & Nommsen-Rivers, L.A. (2014). In-Hospital Formula Use Increases Early Breastfeeding Cessation Among First-time Mothers Intending to Exclusively Breastfeed. The Journal of Pediatrics,164(6). https://doi.org/10.1016/j.jpeds.2013.12.035
- Meek, J., & Noble, L. (2022). Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics, 150(1). https://doi.org/10.1542/peds.2022-057988
- Bartick, M., Stuebe, A., Shealy, K. R., Walker, M., & Grummer-Strawn, L. M. (2009). Closing the Quality Gap: Promoting Evidence-Based Breastfeeding Care in the Hospital- PubMed. Pediatrics, 124(4). https://doi.org/10.1542/peds.2009- 0430
- Niño, D. F., Sodhi, C. P., & Hackam, D. J. (2016). Necrotizing enterocolitis: New insights into pathogenesis and mechanisms. Nature Reviews. Gastroenterology & Hepatology, 13(10). https://doi.org/10.1038/nrgastro.2016.119
- Shulhan, J., Dicken, B., Hartling, L., & Larsen, B. M. (2017). Current Knowledge of Necrotizing Enterocolitis in Preterm Infants and the Impact of Different Types of Enteral Nutrition Products. Advances in Nutrition, 8(1). https://doi.org/10.3945/an.116.013193
- Cristofalo, E. A., Schanler, R. J., Blanco, C. L., Sullivan, S., Trawoeger, R., Kiechl-Kohlendorfer, U., Dudell, G., Rechtman, D. J., Lee, M. L., Lucas, A., & Abrams, S. (2013). Randomized Trial of Exclusive Human Milk Versus Preterm Formula Diets in Extremely Premature Infants – PubMed. The Journal of Pediatrics, 163(6). https://doi.org/10.1016/j.jpeds.2013.07.011
- Bartick, M. C., Schwarz, E. B., Green, B. D., Jegier, B. J., Reinhold, A. G., Colaizy, T. T., Bogen, D. L., Schaefer, A. J., & Stuebe, A. M. (2017). Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs. Maternal & Child Nutrition, 13(1), e12366. https://doi.org/10.1111/mcn.12366
- Ip, S., Chung, M., Raman, G., Chew, P., Magula, N., DeVine, D., Trikalinos, T., & Lau, J. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evidence Report/Technology Assessment, 153. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4781366/
- Collaborative Group on Hormonal Factors in Breast Cancer. (2002). Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50 302 women with breast cancer and 96 973 women without the disease – PubMed. Lancet (London, England), 360(9328). https://doi.org/10.1016/S0140-6736(02)09454-0
- Boquien, C.-Y. (2018). Human Milk: An Ideal Food for Nutrition of Preterm Newborn. Frontiers in Pediatrics, 6. https://doi.org/10.3389/fped.2018.00295
- La Leche League Canada. (n.d.). Mammal Milk Composition and Mothering Styles. La Leche League Canada – Breastfeeding Support and Information. https://www.lllc.ca/mammal-milk-composition-andmothering-styles
- Pietrzak-Fiećko, R., & Kamelska-Sadowska, A. M. (2020). The Comparison of Nutritional Value of Human Milk with Other Mammals’ Milk. Nutrients, 12(5). https://doi.org/10.3390/nu12051404
- Langer, P. (2009). Differences in the Composition of Colostrum and Milk in Eutherians Reflect Differences in Immunoglobulin Transfer. Journal of Mammalogy,90(2), 332–339. https://doi.org/10.1644/08-MAMM-A-071.1
- Lönnerdal, B., Georgieff, M. K., & Hernell, O. (2015). Developmental Physiology of Iron Absorption, Homeostasis and Metabolism in the Healthy Term Infant. The Journal of Pediatrics, 167(4 0). https://doi.org/10.1016/j.jpeds.2015.07.014
- Hegar, B., Wibowo, Y., Basrowi, R. W., Ranuh, R. G., Sudarmo, S. M., Munasir, Z., Atthiyah, A. F., Widodo, A. D., Supriatmo, Kadim, M., Suryawan, A., Diana, N. R., Manoppo, C., & Vandenplas, Y. (2019). The Role of Two Human Milk Oligosaccharides, 2′-Fucosyllactose and Lacto-N-Neotetraose, in Infant Nutrition. Pediatric Gastroenterology, Hepatology & Nutrition, 22(4). https://doi.org/10.5223/pghn.2019.22.4.330
- National Health Service. (2021, June 9). How long do babies carry their mother’s immunity? NHS. https://www.nhs.uk/common-healthquestions/childrenshealth/how-long-do-babies-carry-their-mothers-immunity/
- Goldman, A. S., Garza, C., Nichols, B. L., & Goldblum, R. M. (1982). Immunologic factors in human milk during the first year of lactation. The Journal of Pediatrics, 100(4), 563–567. https://doi.org/10.1016/s0022-3476(82)80753-1
- Goldblum, R. M., Ahlstedt, S., Carlsson, B., Hanson, L. Å., Jodal, U., Lidin Janson, G., & Sohl-Åkerlund, A. (1975). Antibody-forming cells in human colostrum after oral immunisation. Nature, 257(5529), 797–799. https://doi.org/10.1038/257797a0
- Campbell, B., Sarwar, M., & Petersen, W. E. (1957). Diathelic Immunization— a Maternal-Offspring Relationship Involving Milk Antibodies. Science, 125(3254), 932–933. https://doi.org/10.1126/science.125.3254.932
- Goldman, A. S., Garza, C., Nichols, B. L., & Goldblum, R. M. (1982a). Immunologic factors in human milk during the first year of lactation. The Journal of Pediatrics, 100(4), 563–567. https://doi.org/10.1016/s0022-3476(82)80753-1
- Ramírez, D. S. R., Pérez, M. M. L., Pérez, M. C., Hernández, M. I. S., Pulido, S. M., Villacampa, L. P., Vilar, A. M. F., Falero, M. R., Carretero, P. G., Millán, B. R., Roper, S., & Bello, M. Á. G. (2021). SARS-CoV-2 Antibodies in Breast Milk After Vaccination PubMed. Pediatrics, 148(5). https://doi.org/10.1542/peds.2021-052286
- Department of Health, Education, and Welfare. (1979). Trends in Breast Feeding Among American Mothers (Series 23 No. 3). Department of Health, Education, and Welfare, Office of Health Research, Statistics, and Technology National Center for Health Statistics.
https://www.cdc.gov/nchs/data/series/sr_23/sr23_003.pdf - International Vaccine Access Center & Johns Hopkins Bloomberg School of Public Health. (2022). Pneumonia and Diarrhea Progress Report 2022. https://www.jhsph.edu/ivac/wpcontent/uploads/2019/10/PDPR_2022.pdf
- Jelliffe, D. B., MD. (1989). Foreword. In Lactation Forms: A Guide to Lactation Consultant Charting. The Lactation Institute Press.
- Centers for Disease Control and Prevention. (2023). Breastfeeding Report Card: United States, 2022. https://www.cdc.gov/breastfeeding/pdf/2022-Breastfeeding-Report-Card-H.pdf
- Marmet, C.G., & Shell, E.P. (1984). Training Neonates to Suck Correctly. MCN. The American journal of maternal child nursing, 9(6), 401–407. https://doi.org/10.1097/00005721-198411000-00009
- Marmet, C., & Shell, E. (2022). Therapeutic Positioning for Breastfeeding. In Supporting Sucking Skills in Breastfeeding Infants (pp. 495–512). Jones & Bartlett Learning.
- Marmet, C.G., Shell, E.P., with inset by Marmet, R., M.D. (1990). Neonatal Frenotomy May be Necessary to Correct Breastfeeding Problems. Journal of Human Lactation, 6(3).
- IBLCE. (2017, May 17). Current Statistics on Worldwide IBCLCS. IBLCE. https://iblce.org/about-iblce/currentstatistics-on-worldwide-ibclcs
Appendix E
A Pediatric Dentist’s Personal
Journey to Wellness
Appendix E References
- Inda, Michael J. (1981). The Ability of Standard Cephalometric Techniques to Determine Accurately Repositioning of the Hyoid Bone Through the Use of a Tongue crib. Master’s Thesis. Loyola University Chicago
- Cleall, J. F., “Deglutition: A Study of Form and Function,” American Journal of Orthodontics., 51:566-594, Aug., 1965
- Cuozzo, G. S., and Bowman, D. C., “Hyoid positioning During Deglutition Following Forced Positioning of the Tongue,” American Journal of Orthodontics., 68:564-570, Nov., 1975
- Abate, A. et al., “Relationship between Breastfeeding and Malocclusion: A Systematic Review of the Literature,” Nutrients., 12(12),3688 Nov., 2020
- Stecco, C., Functional Atlas of the Human Fascial System, Elsevier, 2015
- www.babylase.com
- Bronson, J. et al, “Introducing the Advanced LightForce (ALF) Appliance,” Oralhealth, March 2015
- Bronson, J. et al, “Introducing the Advanced LightForce (ALF) Appliance,” Oralhealth, March 2015
- Bronson, J. et al, “Introducing the Advanced LightForce (ALF) Appliance,” Oralhealth, March 2015
- Saccomanno S and Paskay, L., New Trends in Myofunctional Therapy, CTG srl – Gorgonzola (MI), Italy, 2020
Appendix F
Tongue-Ties, Lip-Ties, Buccal-Ties:
It Takes a Village

fig. 1, infant visible anterior tongue-tie
fig. 2, tongue tie
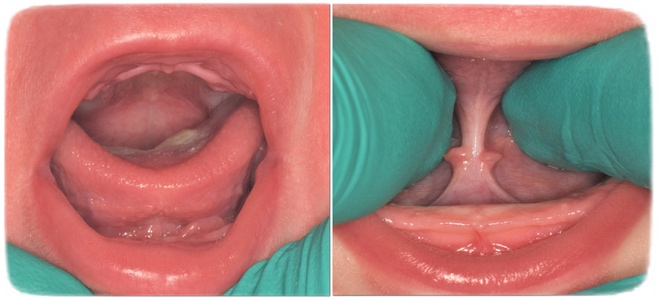
fig.1, infant not visible posterior tongue tie
fig.2, infant posterior tongue-tie revealed

Infant Upper Lip-Tie

Upper Lip-Tie

Buccal-tie
Appendix F References
- https://www.youtube.com/watch?v=Sk5qsmRyVcE&ab_channel=AAPMD
- Ghaheri, B. A., Cole, M., Fausel, S. C., Chuop, M., & Mace, J. C. (2016). Breastfeeding Improvement Following Tongue-Tie and Lip-Tie Release. The Laryngoscope. https://doi.org/10.1002/(issn)1531-4995
- Siegel, S. A. (2016). Aerophagia induced reflux in breastfeeding infants with ankyloglossia and shortened maxillary labial frenula (tongue and lip tie). International Journal of Clinical Pediatrics, 5(1), 6–8. https://doi.org/10.14740/ijcp246w
Appendix G
The Bones Are the Footprints of the Living Anatomy:
Osteopathic Treatment and Myofunctional Therapy
Appendix G References
- Still A. T. Autobiography. Newark, OH. American Academy of Osteopathy. reprint, 1989, p.142.
- American Osteopathic Association. Resolution 608: Tenets of Osteopathic Medicine. Chicago, IL. Reafirmed, July, 2023.
- Still, C. Letter to Ray Hurlburt, President of the AOA. Collection of the Still National Osteopathic Museum, Kirksville, MO. September 4, 1940.
- https://cranialacademy.org/research/analysis/
- England, M A. Life Before Birth. London: Mosby-Wolfe. 1996. p.84.
- Seeds A. E. Current Concepts of Amniotic Fluid Dynamics. Am Journal of Obset Gynecol. 1980. 138:575,
- Still, A T. Lecture Notes: Tongue. Collection of the Still National Osteopathic Museum, Kirksville, MO. c1907.
Appendix H
Functional Breathing for Sleep, Mood, and Health
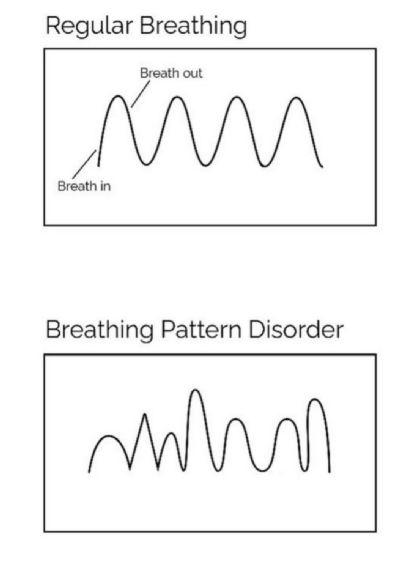
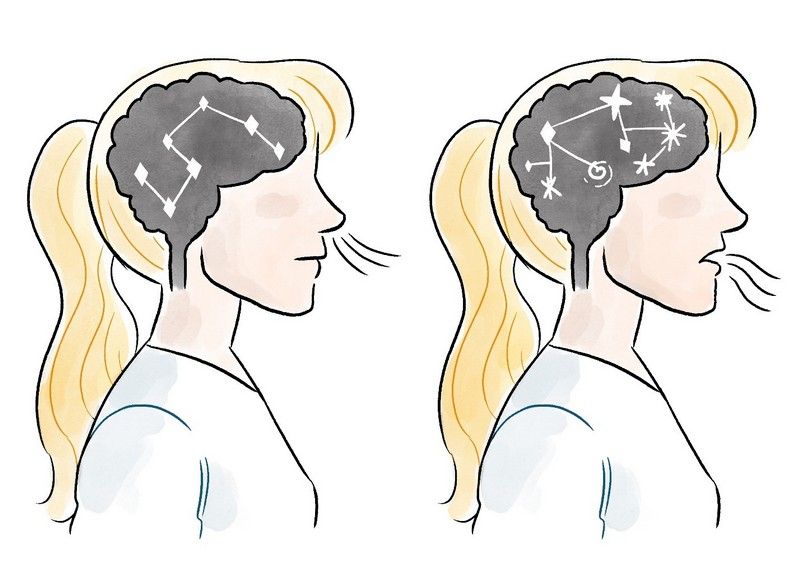
© Patrick McKeown Breathing pattern disorder
© Patrick McKeown Breathing pattern disorder
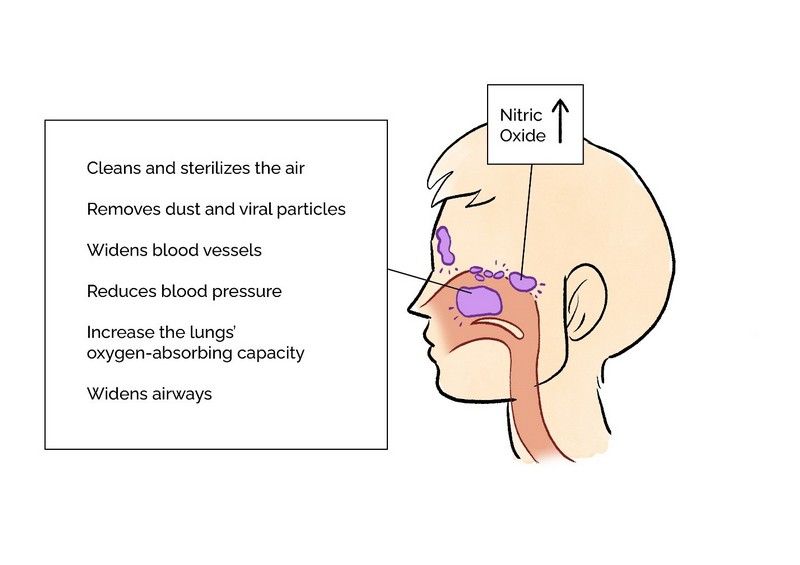
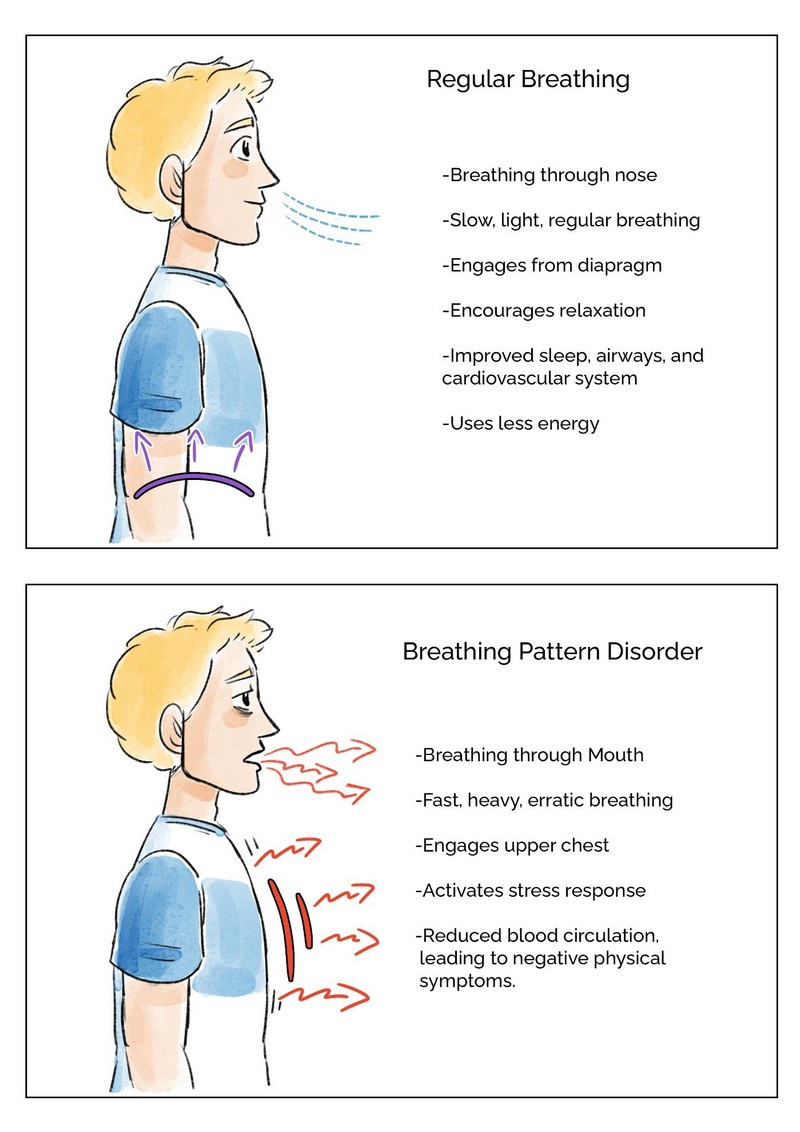
© Patrick McKeown Proper breathing
© Patrick McKeown Meditative breathing
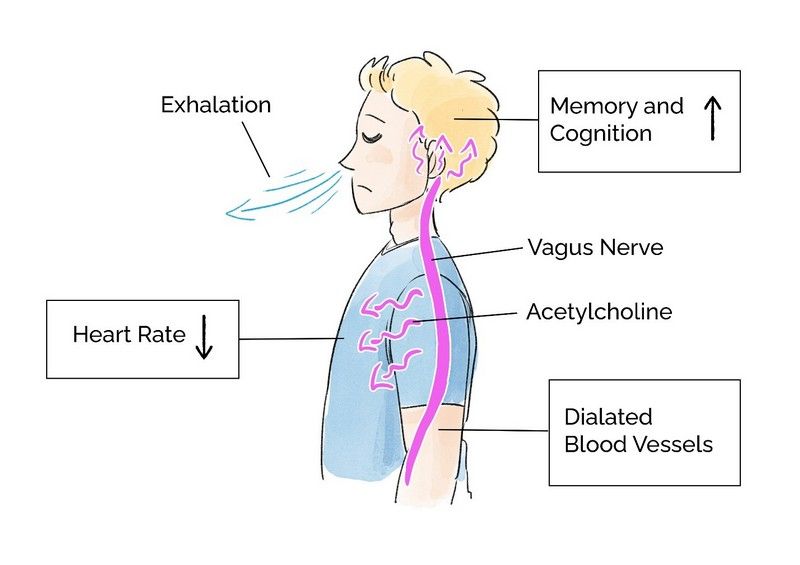
© Patrick McKeown Vagus nerve, acetylcholine
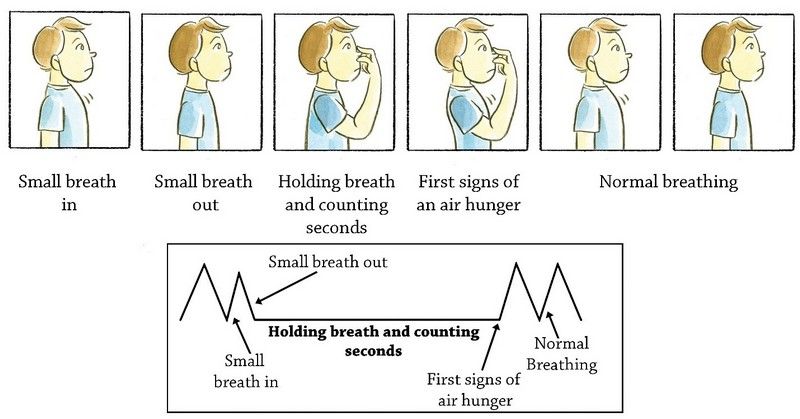
© Patrick McKeown Control pause breathing
© Patrick McKeown Control pause breathing
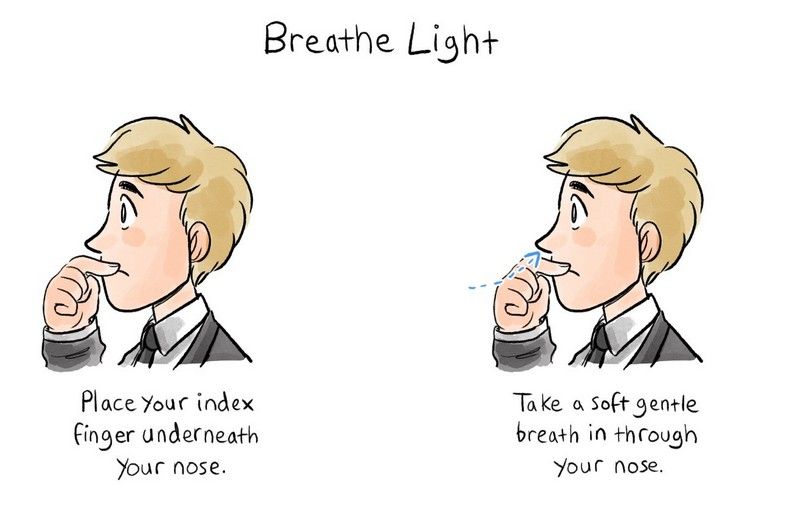
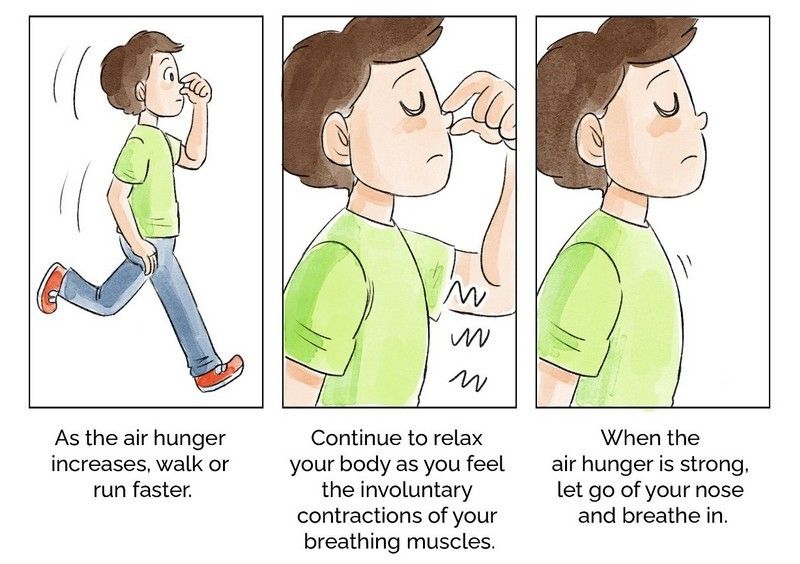
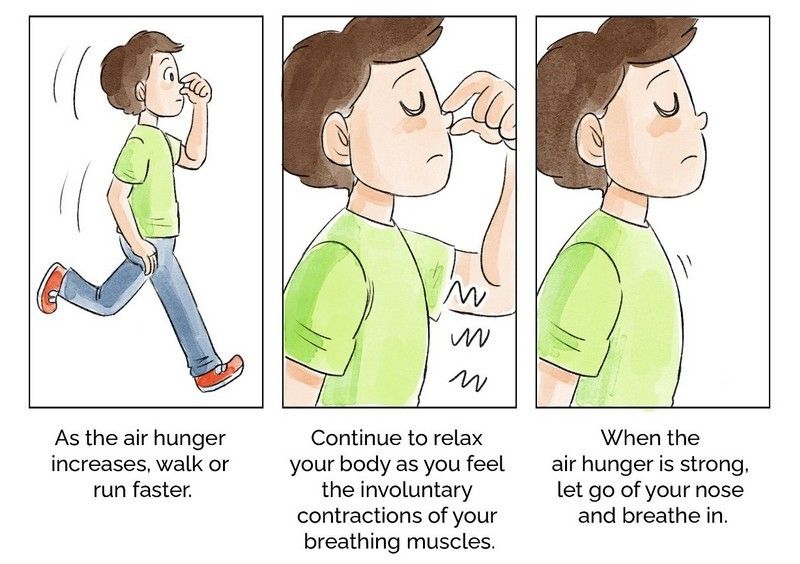
Breathe light exercise
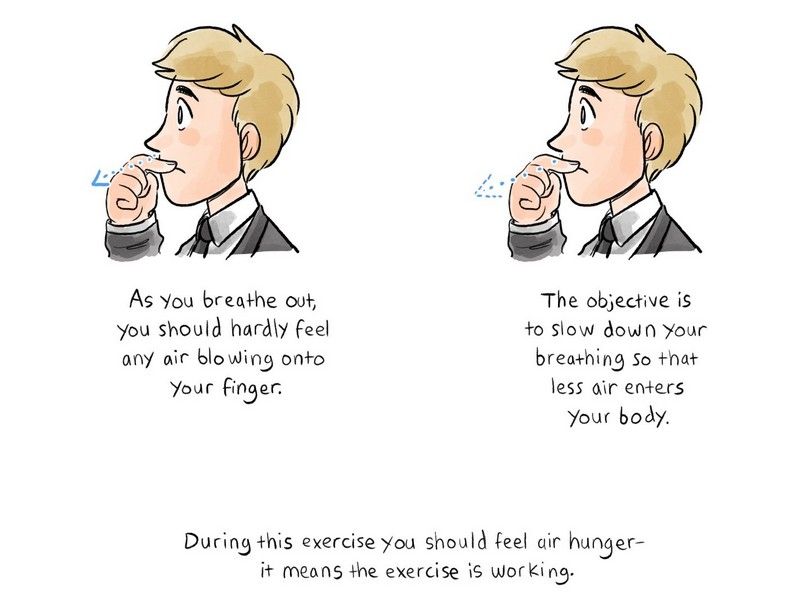
© Patrick McKeown Breathe light
© Patrick McKeown children’s breathing assessment
© Patrick McKeown
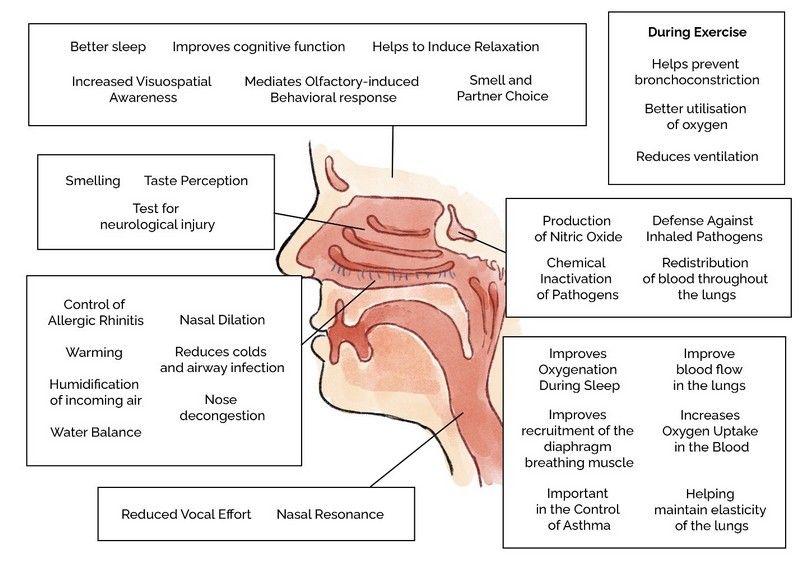
© Patrick McKeown Benefits
Appendix H References
- Michael Gibson, Farman Khan, Hyperventilation Syndrome epidemiology and demographics.
- Thomas, M., McKinley, R. K., Freeman, E., & Foy, C. (2001). Prevalence of dysfunctional breathing in patients treated for asthma in primary care: cross sectional survey. Bmj, 322(7294), 1098-1100.
- Thomas, M., McKinley, R. K., Freeman, E., Foy, C., & Price, D. (2005). The prevalence of dysfunctional breathing in adults in the community with and without asthma. Primary care respiratory journal : journal of the General Practice Airways Group, 14(2), 78–82.
- Martinez-Moragon E, Perpina M, Belloch A, Prevalence of hyperventilation syndrome in patients treated for asthma in a pulmonology clinic, 2005.
- Morton E. Tavel, Hyperventilation Syndrome: A Diagnosis Usually unrecognized, May 10, 2017.
- Spinhoven P et. Al., Hyperventilation and panic attacks in general hospital patients, 1993.
- https://londonchestspecialist.co.uk/2021/11/03/dysfunctionalbreathing-what-is-it-and-how-can-i-manage-it/. Accessed 23/03/23.
- https://www.buteykobreathing.nz/blog/nasal-diaphragmbreathing. Accessed 23/03/23.
- Video Translation of Professor Buteyko from ButeykoClinic.com, Buteyko Clinic, Moscow, 2007.
- The Life of Konstantin Pavlovich Buteyko, Buteyko Clinic International.
- Mendonca, K. M., Freitas, D. A., Macedo, T. M., Silva, A. C., Amaral, C. T., Santino, T. A., & McKeown, P. (2017). Buteyko method for children with asthma: A randomized controlled trial. In A66. THE MANY FACES OF ASTHMA IN CHILDHOOD (pp. A2203-A2203). American Thoracic
Society. - Cowie, R. L., Conley, D. P., Underwood, M. F., & Reader, P. G. (2008). A randomised controlled trial of the Buteyko technique as an adjunct to conventional management of asthma. Respiratory medicine, 102(5), 726-732.
- Prasanna, K. B., Sowmiya, K. R., & Dhileeban, C. M. (2015). Effect of Buteyko breathing exercise in newly diagnosed asthmatic patients. International Journal of Medicine and Public Health, 5(1).
- Meuret, Alicia E., David Rosenfield, Anke Seidel, Lavanya Bhaskara, and Stefan G. Hofmann. “Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity.” Journal of consulting and clinical psychology 78, no. 5 (2010): 691.
- Fitzpatrick MF1, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
- Chang HR (2011) Nitric Oxide, the Mighty Molecule: Its Benefits for Your Health and Well-being, Jacksonville, FL: The Mind Society.
- De Groote, M. A., & Fang, F. C. (1995). NO inhibitions: antimicrobial properties of nitric oxide. Clinical Infectious Diseases, 21(Supplement_2), S162-S165.
- Hermann, M., Flammer, A., & Lüscher, T. F. (2006). Nitric oxide in hypertension. The Journal of Clinical Hypertension, 8, 17-29.
- Ignarro, L. (2006). NO More Heart Disease: How Nitric Oxide Can Prevent–Even Reverse–Heart Disease and Strokes. St. Martin’s Press.
- J.O. Lundberg et al. Inhalation of Nitric oxide modulates pulmonary function in humans, December, 1996.
- Allen, R. The health benefits of nose breathing. Nursing in General Practice. 2015-01.
- Russo MA, Santarelli DM, O’Rourke D. The physiological effects of slow breathing in the healthy human. Breathe (Sheff). 2017 Dec;13(4):298-309.
- Richard St John, 8 Secrets of Success, TED Talk, 2005. https://youtu.be/UN79-Tv5GHY.
- Cottle, M.H., 1987. The work, ways, positions and patterns of nasal breathing (relevance in heart and lung illness). Reprinted in: Barelli, P., Loch, W.E.E., Kern, E.R., Steiner, A. (Eds.), Rhinology. The collected writings of Maurice H. Cottle, MD.
- Lee K.J et.al. EEG Signals during Mouth Breathing in a Working Memory Task, 2019.
- Ma, X., Yue, Z. Q., Gong, Z. Q., Zhang, H., Duan, N. Y., Shi, Y. T., Wei, G. X., & Li, Y. F. (2017). The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Frontiers in psychology, 8, 874.
- Jung, J. Y., & Kang, C. K. (2021). Investigation on the Effect of Oral Breathing on Cognitive Activity Using Functional Brain Imaging. Healthcare (Basel, Switzerland), 9(6), 645.
- Zelano, C., Jiang, H., Zhou, G., Arora, N., Schuele, S., Rosenow, J., & Gottfried, J. A. (2016). Nasal respiration entrains human limbic oscillations and modulates cognitive function. Journal of Neuroscience, 36(49), 12448-12467.
- “Rhythm of Breathing Affects Memory and Fear.” Neuroscience News. (December 7, 2016). http://www.neurosciencenews.com/memory-fear-breathing-5699/ (Accessed July 14, 2022).
- Eugene, A. R., & Masiak, J. (2015). The Neuroprotective Aspects of Sleep. MEDtube science, 3(1), 35–40.
- Ma, X., Yue, Z. Q., Gong, Z. Q., Zhang, H., Duan, N. Y., Shi, Y. T., Wei, G. X., & Li, Y. F. (2017). The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Frontiers in psychology, 8, 874.
- Bonuck, K., Freeman, K., Chervin, R. D., & Xu, L. (2012). Sleep-disordered breathing in a population-based cohort: behavioral outcomes at 4 and 7 years. Pediatrics, 129(4), e857–e865.
- Jung, J. Y., & Kang, C. K. (2021, May). Investigation on the Effect of Oral Breathing on Cognitive Activity Using Functional Brain Imaging. In Healthcare (Vol. 9, No. 6, p. 645). MDPI.
- Trosman I, Trosman SJ. Cognitive and Behavioral Consequences of Sleep Disordered Breathing in Children. Med Sci (Basel). 2017 Dec 1;5(4):30.
- CW Zwillich et.al., Disturbed Sleep and Prolonged Apnea During Nasal Obstruction in Normal Men, 1981.
- Hiroko Tsuda et.al., The relationship between mouth opening and sleep stage-related sleep disordered breathing, 2011.
- Olsen KD, Kern EB, Westbrook PR. Sleep and breathing disturbance secondary to nasal obstruction. Otolaryngol Head Neck Surg. 1981 Sep-Oct;89(5):804-10.
- Fitzpatrick MF1, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
- McKeown, P., O’Connor-Reina, C., & Plaza, G. (2021). Breathing Re-Education and Phenotypes of Sleep Apnea: A Review. Journal of clinical medicine, 10(3), 471.
- https://www.who.int/news-room/questions-andanswers/item/stress (accessed 24/03/23).
- Buteyko Clinic, Mouth Breathing Causes, Treatment and Consequences, October 12, 2020.
- https://med.stanford.edu/news/all-news/2017/03/studydiscovers-how-slow-breathing-induces-tranquility.html
- Kiesel K, Rhodes T, Mueller J, Waninger A, Butler R. Development of A Screening Protocol to Identify Individuals With Dysfunctional Breathing. Int J Sports Phys Ther. 2017 Oct;12(5):774-786. PMID: 29181255; PMCID: PMC5685417.
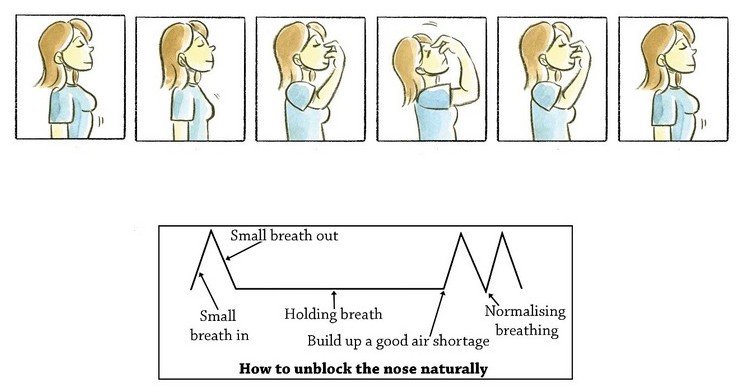
- Harley Street Clinic, Can Breathing Exercises Help with Nose Blocks? January 31, 2020.
- Patrick McKeown, Breathe Light to Breathe Right, 2023.
Appendix I
Thirty Functions of the Nose
Appendix I References
-
- Russo MA, Santarelli DM, O’Rourke D. The physiological effects of slow breathing in the healthy human. Breathe (Sheff). 2017;13(4):298-309. doi:10.1183/20734735.009817
- Soler ZM, Eckert MA, Storck K, Schlosser RJ (2015) Cognitive function in chronic rhinosinusitis: a controlled clinical study. Int Forum Allergy Rhinol. 5(11):1010–1017
- Ihara, Yasuo, et al. “HLA and human mate choice: tests on Japanese couples.” Anthropological Science 108.2 (2000): 199-214.
- Bergland, Christopher. “Breathe In! Nasal Inhalations Are Linked to Laser-Like Focus.” Weizmann Institute of Science. Published March 17, 2019. www.weizmann-usa.org/news-media/in-the-news/breathe-in-nasal-inhalations-are-linked-to-laser-like-focus (accessed January 7, 2020).
Perl, Ofer, Aharon Ravia, Mica Rubinson, Ami Eisen, Timna Soroka, Nofar Mor, Lavi Secundo, and Noam Sobel. “Human non-olfactory cognition phase-locked with inhalation.” Nature human behaviour 3, no. 5 (2019): 501. - Kadohisa M. Effects of odor on emotion, with implications. Front Syst Neurosci. 2013;7:66. Published 2013 Oct 10. doi:10.3389/fnsys.2013.00066
- Sivasankar M, Fisher KV. Oral breathing increases Pth and vocal effort by superficial drying of vocal fold mucosa. J Voice. 2002 Jun;16(2):172-81. doi:10.1016/s0892-1997(02)00087-5. PMID: 12150370
- Young A, Spinner A. Velopharyngeal Insufficiency. 2023 Jan 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 33085296.
- Trevisan ME, Boufleur J, Soares JC, Haygert CJ, Ries LG, Corrêa EC. Diaphragmatic amplitude and accessory inspiratory muscle activity in nasal and mouth-breathing adults: a cross-sectional study. J Electromyogr Kinesiol. 2015 Jun;25(3):463-8. doi:10.1016/j.jelekin.2015.03.006. Epub 2015 Apr 6. PMID: 25900327.
- Swift AC, Campbell IT, McKown TM. Oronasal obstruction, lung volumes, and arterial oxygenation. Lancet. 1988 Jan 16;1(8577):73-5. doi:10.1016/s0140-6736(88)90282-6. PMID: 2891980.
- Lundberg JO, Settergren G, Gelinder S, Lundberg JM, Alving K, Weitzberg E. Inhalation of nasally derived nitric oxide modulates pulmonary function in humans. Acta Physiol Scand. 1996 Dec;158(4):343-7. doi:10.1046/j.1365-201X.1996.557321000.x. PMID: 8971255
- Lundberg JO,Settergren G,Gelinder S,Lundberg JM,Alving K,Weitzberg E. 1996d. Inhalation of nasally derived nitric oxide modulates pulmonary function in humans. Acta Physiol Scand 158: 343–347.
- Sánchez Crespo A, Hallberg J, Lundberg JO, Lindahl SG, Jacobsson H, Weitzberg E, Nyrén S. Nasal nitric oxide and regulation of human pulmonary blood flow in the upright position. J Appl Physiol (1985). 2010 Jan;108(1):181-8. doi:10.1152/japplphysiol.00285.2009. Epub
2009 Oct 29. PMID: 19875719.
Bartley J., Wong C. (2013) Nasal Pulmonary Interactions. In: Önerci T. (eds) Nasal Physiology and Pathophysiology of Nasal Disorders. Springer, Berlin, Heidelberg. - Andrew B Lumb MB BS FRCA, in Nunn’s Applied Respiratory Physiology (Eighth Edition), 2017
Nonrespiratory (https://www.sciencedirect.com/science/article/pii/B9780702062940000113) Functions of the Lung (https://www.sciencedirect.com/science/article/pii/B9780702062940000113). Andrew B Lumb MB BS FRCA, in Nunn’s Applied Respiratory Physiology (Eighth Edition) (https://www.sciencedirect.com/book/9780702062940/nunns-applied-respiratory-physiology), 2017
Ritz T, Trueba AF, Vogel PD, Auchus RJ, Rosenfield D. Exhaled nitric oxide and vascular endothelial growth factor as predictors of cold symptoms after stress. Biol Psychol 2018;132:116e24. - https://www.sciencedirect.com/topics/medicine-and-dentistry/nasal-breathing Accessed: 29th March 2023
- Widdicombe J. Microvascular anatomy of the nose. Allergy. 1997;52(40 Suppl):7-11. doi:10.1111/j.1398-9995.1997.tb04877.x. PMID: 9353554. Geurkink N. Nasal anatomy, physiology, and function. J Allergy Clin Immunol. 1983 Aug;72(2):123-8. doi:10.1016/0091-6749(83)90518-3. PMID: 6350406.
- Naclerio RM, Pinto J, Assanasen P, Baroody FM. Observations on the ability of the nose to warm and humidify inspired air. Rhinology. 2007 Jun;45(2):102-11. PMID: 17708456. Rundell KW, Jenkinson DM. Exercise-induced bronchospasm in the elite athlete. Sports Med. 2002;32(9):583-600. doi:10.2165/00007256-200232090-00004. PMID: 12096931.
- Svensson S, Olin AC, Hellgren J. Increased net water loss by oral compared to nasal expiration in healthy subjects. Rhinology. 2006 Mar;44(1):74-7. PMID: 16550955.
- Hsu YB, Lan MY, Huang YC, Kao MC, Lan MC. Association Between Breathing Route, Oxygen Desaturation, and Upper Airway Morphology. Laryngoscope. 2021 Feb;131(2):E659-E664. doi:10.1002/lary.28774. Epub 2020 May 30. PMID: 32473063.
- Olsen KD, Kern EB, Westbrook PR. Sleep and breathing disturbance secondary to nasal obstruction. Otolaryngol Head Neck Surg. 1981 Sep-Oct;89(5):804-10. doi:10.1177/019459988108900522. PMID: 6799913.)
Petruson B. Increased nasal breathing decreases snoring and improves oxygen saturation during sleep apnoea. Rhinology. 1994 Jun;32(2):87-9. PMID: 7939149. - Nagappan PG, Subramaniam S, Wang DY. Olfaction as a soldier– a review of the physiology and its present and future use in the military. Mil Med Res. 2017 Mar 15;4:9. doi:10.1186/s40779-017-0119-4. PMID: 28344819; PMCID: PMC5359863.
Gillman GS, Bakeman AE, Soose RJ, Wang EW, Schaitkin BM, Lee SE, Chang YF, Mims MM. Will nasal airway surgery improve my sense of smell? A prospective observational study. Int Forum Allergy Rhinol. 2022 Nov 22. doi:10.1002/alr.23115. Epub ahead of print. PMID: 36413461 - Ruff RL, Riechers RG 2nd, Wang XF, Piero T, Ruff SS. A case-control study examining whether neurological deficits and PTSD in combat veterans are related to episodes of mild TBI. BMJ Open. 2012 Mar 18;2(2):e000312. doi:10.1136/bmjopen-2011-000312. PMID: 22431700; PMCID: PMC3312078.
- Rolls ET. Taste, olfactory, and food reward value processing in the brain. Prog Neurobiol. 2015 Apr;127-128:64-90. doi:10.1016/j.pneurobio.2015.03.002. Epub 2015 Mar 23. PMID: 25812933.
- Peterson B, Theman K. Reduced nocturnal asthma by improved nasal breathing. Acta Otolaryngol. 1996 May;116(3):490-2. doi:10.3109/00016489609137878. PMID: 8790753.
- Widdicombe J. Microvascular anatomy of the nose. Allergy. 1997;52(40 Suppl):7-11. doi:10.1111/j.1398-9995.1997.tb04877.x. PMID: 9353554.
- Hasegawa M, Kern EB. The effect of breath holding, hyperventilation, and exercise on nasal resistance. Rhinology. 1978 Dec;16(4):243-9.
DURING PHYSICAL EXERCISE
-
- Otolaryngol Head Neck Surg. 1984 Jun;92(3):302-7.Role of the nasal airway in regulation ofairway resistance during hypercapnia and exercise. Second-Place Resident Award at 1982 Research Forum.
- Shturman-Ellstein R, Zeballos RJ, Buckley JM, Souhrada JF. The beneficial effect of nasalbreathing on exercise-induced bronchoconstriction. Am Rev Respir Dis. 1978 Jul;118(1):65-73. doi:10.1164/arrd.1978.118.1.65. PMID: 677559.
- Morton, A. R., K. King, S. Papalia, Carmel Goodman, K. R. Turley, and J. H. Wilmore. “Comparison of maximal oxygen consumption with oral and nasal breathing.” Australian journal of science and medicine in sport 27, no. 3 (1995): 51-55.
- Dallam, George M., Steve R. McClaran, Daniel G. Cox, and Carol P. Foust. “Effect of Nasal Versus Oral Breathing on Vo2max and Physiological Economy in Recreational Runners Following an Extended Period Spent Using Nasally Restricted Breathing.” International
Journal of Kinesiology and Sports Science 6, no. 2 (2018): 22-29.
NOSE BREATHING FOR FACIAL DEVELOPMENT
- Baumann I, Plinkert PK. Der Einfluss von Atemmodus und Nasenventilation auf das Gesichtsschädelwachstum [Effect of breathing mode and nose ventilation on growth of the facial bones]. HNO. 1996 May;44(5):229-34. German. PMID: 8707626.
Appendix J
Orthodontics and Myofunctional Therapy: Then, Now, and Preferred Future

Dr. Bill Hang (77) Running the Boston Marathon With Mouth Taped To Encourage Nose Breathing
Appendix J References
-
- Catlin, G, 1882 “Shut Your Mouth and Save Your Life”, London, Trubner & Co., 57 & 59, Ludgate Hill.
- Dickens, C, The posthumous papers of the Pickwick Club, OL 23001437M (https://openlibrary.org/books/OL23001437M).
- Bowman, GF, Dental Cosmos.
- Bogue, EA. Orthodontia on the deciduous teeth. The Dental Digest. 1912: no 10,11,12. 1913; no 1,2,3,4,5,7,8.
- Tweed, C, Charles H. Tweed International Foundation For Orthodontic Research and Education: The Tweed Years; www.tweedortho.com.
- Price,W, “Nutrition and Physical Degeneration”, 1939, New York: Paul B Hoeber.
- Mew, J, “The Cause and Cure of Malocclusion, Published by John Mew, Braylsham Castle, Broad Oak, Heathfield. United Kingdom. 2013.
- Mew, J, 2004, “The Postural Basis of Malocclusion: A philosophical overview”. American Journal of Orthodontics and Dentofacial Orthopedics.
- Mew, J, “The aeteology of malocclusion: can the Tropic Premise assist our understanding”, 1981 British Dental Journal 151; :296-302.
- Singh, G, Garcia-Motta,A.V., Hang, W, “Evaluation of the Posterior Airway Space Following
- Hang W, Gelb M, “Airway Centric® TMJ philosophy/Airway Centric® orthodontics ushers in the postretraction world of orthodontics”, Cranio. 2017 Mar; 35(2):68-78.
- Annual Reports and Resolutions, 158th ADA Annual Session, Atlanta, GA, October 19-23, 2017.
- Harper, R, “Sleep apnea linked to brain damage”, American Psychological Association, Feb 2003, Vol 34, Number 2.
- Bonuck K, et al, “Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 Years, Pediatrics 2012 April; 129(4):e857-e865.
- Kheirandish-Gozal L, et al, “Regional brain tissue integrity in pediatric obstructive sleep apnea, Neurosci Lett, 2018 Aug 24;682:118-123.
- Gozal, D, AACP lecture, Scottsdale, AZ.
- McNamara J, “Components of Class II Malocclusion in Children 8-10 Years of Age, The Angle Orthodontist, Vol 51 No 3, July 1981, 177-202.
- Trenouth, MJ, Desoral, SR, How many teeth are extracted as part of orthodontic treatment? A survey of 2038 UK Residents,International Journal of Dentistry and Oral Science,(IJDOS) ISSN: 2377-8075.
Appendix K
Sleep Well, Live Well: Personal Perspectives of a Sleep Medicine Doctor

Figure 1: Anatomy of the pharynx. Note that the low position of the posterior tongue and loss of contact between the soft palate and tongue is how the pharynx looks in cadavers but is abnormal as a resting posture in living humans.
Adapted from Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Image is free to use with attribution under a Creative Commons copyright license. https://commons.wikimedia.org/wiki/File:Blausen_0861_Tonsils%26Throat_Anatomy2.png
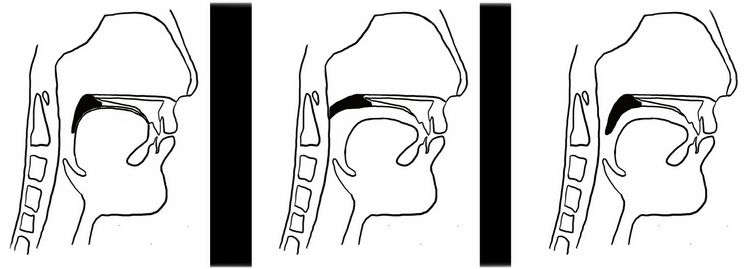
1. Nasal Breathing | 2. Mouth Breathing | 3. Oronasal Breathing
Figure 2: Configuration of the soft palate during nasal breathing, oral breathing, and oronasal breathing. Note that the soft palate forms a seal with the posterior tongue during nasal breathing and forms a seal with the pharyngeal walls during oral breathing, but no seal is formed during oronasal breathing.
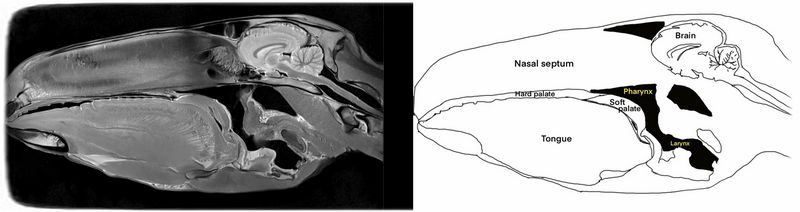
Figure 3: Midsagittal MRI of a horse head, showing the long seal between the soft palate and posterior tongue, which supports nasal breathing. Air in the pharynx shows up black. MRI image was reprinted with the kind permission of Veterinarian Key. https://veteriankey.com/1-overview-of-ct-and-mri-of-theequine-head/
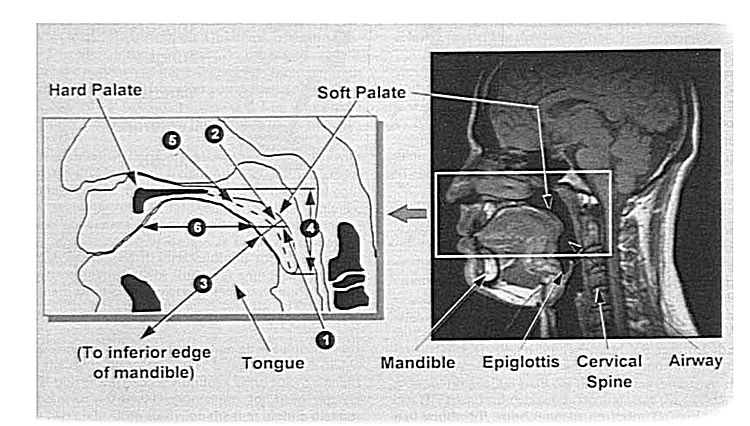
Figure 4: Midsagittal MRI showing the high resting posterior tongue position and long seal between the tongue and soft palate in a normal subject who was confirmed to not have sleep disordered breathing, and had a respiratory disturbance index of < 3 events/hour on overnight polysomnography. The number labels refer to measurements and can be disregarded. From Schwab RJ et al., 1995, Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med. 152(5 Pt 1):1673-89. Reprinted with permission of the American Thoracic Society. Copyright © 2023 American Thoracic Society. All rights reserved. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American
Thoracic Society.
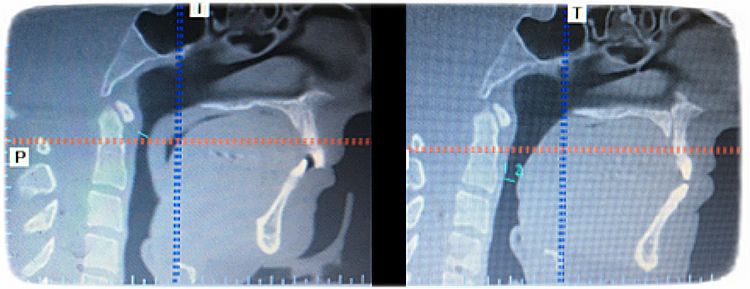
Figure 5: Cone beam CTs of the author before and after myofunctional therapy. Image A on the left shows my resting oropharyngeal posture prior to myofunctional therapy: the soft palate (arrow) is in the oronasal breathing posture, in which air will flow through both the nose and mouth if the lips were parted. Note the black space (air) between the tongue and the soft palate. Image B on the right shows my resting oropharyngeal posture after myofunctional therapy. The soft palate is now creating a seal with the posterior tongue, such that only nasal breathing would occur if the lips were parted. The airspace between the palate and tongue has disappeared. Note also that the
hyoid bone (arrowhead) also moved upwards after myofunctional therapy, showing improved support of the tongue base from the skull.
Appendix K References
- Blumen M, Bequignon E, Chabolle F. Drug-induced sleep endoscopy: A new gold standard for evaluating OSAS? Part II: Results. Eur Ann Otorhinolaryngol Head Neck Dis. 2017 Apr;134(2):109-115.
- Rodenstein DO, Stanescu DC. Soft palate and oronasal breathing in humans. J Appl Physiol Respir Environ Exerc Physiol. 1984 Sep;57(3):651-7.
- Fitzpatrick MF, McLean H, Urton AM, et al. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
- Gleeson K, Zwillich CW, Braier K, et al. Breathing route during sleep. Am Rev Respir Dis. 1986 Jul;134(1):115-20.
- Azarbarzin A, Sands SA, Marques M, et al. Palatal prolapse as a signature of expiratory flow limitation and inspiratory palatal collapse in patients with obstructive sleep apnoea. Eur Respir J. 2018 Feb;51(2).
- Diaferia G, Santos-Silva R, Truksinas E, et al. Myofunctional therapy improves adherence to continuous positive airway pressure treatment. Sleep Breath. 2017 May;21(2):387-395.
- Deacon-Diaz NL, Sands SA, McEvoy RD, et al. Daytime loop gain is elevated in obstructive sleep apnea but not reduced by CPAP treatment. J Appl Physiol (1985). 2018 Nov 1;125(5):1490-1497.
- Yamauchi M, Jacono FJ, Fujita Y, et al. Breathing irregularity during wakefulness associates with CPAP acceptance in sleep apnea. Sleep Breath. 2013 May;17(2):845-52.
- Buterbaugh J, Wynstra C, Provencio N, et al. Cerebrovascular reactivity in young subjects with sleep apnea. Sleep. 2015 Feb 1;38(2):241-50.
- Camacho M, Certal V, Abdullatif J, et al. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. Sleep. 2015 May 1;38(5):669-75.
Figure 1: Adapted from Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Image is free to use with attribution under a Creative Commons copyright license. https://commons.wikimedia.org/wiki/File:Blausen_0861_Tonsils%26Throat_Anatomy2.png
Appendix M
Team Building for the Treatment of Myofunctional Disorders
Appendix M Selected References
- Walther DS. Applied Kinesiology. Synopsis. 2nd edition. 2000. SYSTEMS DC, Puebla CO.
- Walter DS. Applied Kinesiology. Volume II. 1983. SYSTEMS DC, Puebla CO.
- Magoun HI. Osteopathy in the Cranial Field. Third edition. 1976. Magoun (Editor).
- Price WA. Nutrition and Physical Degeneration. 8th Edition. 2009. Price-Pottenger Publisher.
Appendix N
The Theory of Spiky-Leaky Syndrome
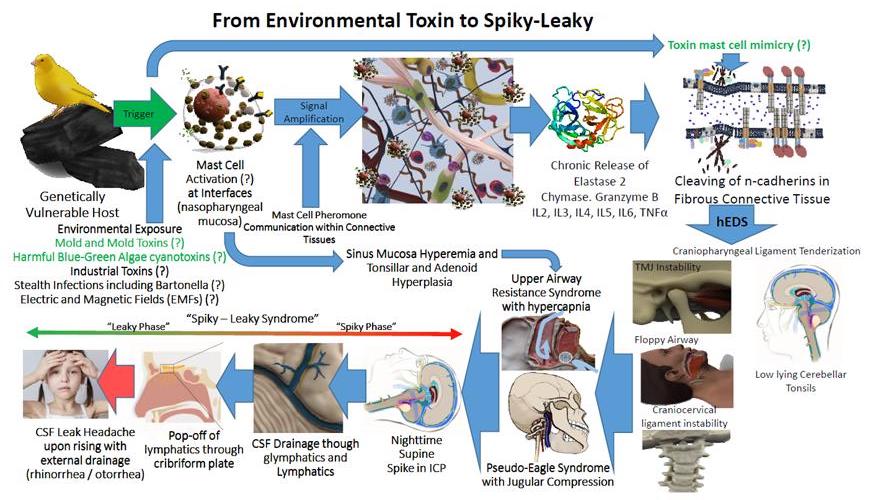
From Environmental Toxin to Spiky-Leaky
Appendix N References
- Maxwell AJ. Dysautonomia. In: Jovin D, editor. Disjointed: Navigating the Diagnosis and Management of hypermobile Ehlers-Danlos Syndrome and Hypermobility Spectrum Disorders. 1st ed. San Francisco: Hidden Stripes Publications, Inc; 2020. p. 134-215.
- Afrin LB, Molderings, G. J. A concise, practical guide to diagnostic assessment for mast cell activation disease World J Hematology. 2014;3(1):1-17.
- Afrin LB, Ackerley MB, Bluestein LS, Brewer JH, Brook JB, Buchanan AD, et al. Diagnosis of mast cell activation syndrome: a global “consensus-2”. Diagnosis (Berl). 2021;8(2):137-52.
- Malfait F, Francomano C, Byers P, Belmont J, Berglund B, Black J, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8-26.
- Miller AJ, Stiles LE, Sheehan T, Bascom R, Levy HP, Francomano CA, et al. Prevalence of hypermobile Ehlers-Danlos syndrome in postural orthostatic tachycardia syndrome. Auton Neurosci. 2020;224:102637.
- Wang E, Ganti T, Vaou E, Hohler A. The relationship between mast cell activation syndrome, postural tachycardia syndrome, and Ehlers-Danlos syndrome. Allergy Asthma Proc. 2021;42(3):243-6.
- Bonamichi-Santos R, Yoshimi-Kanamori K, Giavina-Bianchi P, Aun MV. Association of Postural Tachycardia Syndrome and Ehlers-Danlos Syndrome with Mast Cell Activation Disorders. Immunol Allergy Clin North Am. 2018;38(3):497-504.
- Mao G, Kopparapu S, Jin Y, Davidar AD, Hersh AM, Weber-Levine C, et al. Craniocervical Instability in Patients With Ehlers-Danlos Syndrome: Controversies in Diagnosis and Management. Spine J. 2022.
- Rosa S, Baird, J.W. The Craniocervical Junction: Observations regarding the Relationship between Misalignment, Obstruction of Cerebrospinal Fluid Flow, Cerebellar Tonsillar Ectopia, and Image-Guided Correction. In: Smith FW, Dworkin, J.S., editor. The Craniocervical Syndrome and MRI. Basel: Karger; 2015. p. 48-66.
- Wardly DE. Intracranial hypertension associated with obstructive sleep apnea: a discussion of potential etiologic factors. Med Hypotheses. 2014;83(6):792-7.
- Del Pozzi AT, Schwartz CE, Tewari D, Medow MS, Stewart JM. Reduced cerebral blood flow with orthostasis precedes hypocapnic hyperpnea, sympathetic activation, and postural tachycardia syndrome. Hypertension. 2014;63(6):1302-8.
- Fischer AQ, Chaudhary BA, Taormina MA, Akhtar B. Intracranial hemodynamics in sleep apnea. Chest. 1992;102(5):1402-6.
- Hulens M, Rasschaert R, Vansant G, Stalmans I, Bruyninckx F, Dankaerts W. The link between idiopathic intracranial hypertension, fibromyalgia, and chronic fatigue syndrome: exploration of a shared pathophysiology. J Pain Res. 2018;11:3129-40.
- Wardly D, Wolford LM, Veerappan V. Idiopathic intracranial hypertension eliminated by counterclockwise maxillomandibular advancement: a case report. Cranio. 2017;35(4):259-67.
- Chang ET, Fernandez-Salvador C, Giambo J, Nesbitt B, Liu SY, Capasso R, et al. Tongue retaining devices for obstructive sleep apnea: A systematic review and metaanalysis. Am J Otolaryngol. 2017;38(3):272-8.
- Olivi G, Signore A, Olivi M, Genovese MD. Lingual frenectomy: functional evaluation and new therapeutical approach. Eur J Paediatr Dent. 2012;13(2):101-6.
- Guilleminault C, Huseni S, Lo L. A frequent phenotype for paediatric sleep apnoea: short lingual frenulum. ERJ Open Res. 2016;2(3).
- Yoon A, Zaghi S, Weitzman R, Ha S, Law CS, Guilleminault C, et al. Toward a functional definition of ankyloglossia: validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017;21(3):767-75.
- Koka V, De Vito, A., Roisman, G., Petitjean, M., Giulio Romano, G., Pignatelli, F. Padovani, D., Randerath, W. Orofacial Myofunctional Therapy in Obstructive Sleep Apnea Syndrome: A Pathophysiological Perspective. Medicina. 2021;57(323):1-10.
- Moeller MR. The emerging area of orofacial myofunctional therapy: Efficacy of treatment in sleep disordered breathing bringing promise of a new field of medicine. Cranio. 2018;36(5):283-5.
- Moeller JL. Orofacial myofunctional therapy: why now? Cranio. 2012;30(4):235-6.
- Rogers AP. Exercises for the Development of the Muscles of the Face, with a View to Increasing Their Functional Activity. The Dental cosmos; a monthly record of dental science. 1918;60(1).
- Camacho M, Guilleminault C, Wei JM, Song SA, Noller MW, Reckley LK, et al. Oropharyngeal and tongue exercises (myofunctional therapy) for snoring: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2018;275(4):849-55.
- Bandyopadhyay A, Kaneshiro K, Camacho M. Effect of myofunctional therapy on children with obstructive sleep apnea: a meta-analysis. Sleep Med. 2020;75:210-7.
- Guimaraes KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2009;179(10):962-6.
- Villa MP, Evangelisti M, Martella S, Barreto M, Del Pozzo M. Can myofunctional therapy increase tongue tone and reduce symptoms in children with sleep-disordered breathing? Sleep Breath. 2017;21(4):1025-32.
- Boyd K, Saccomanno S, Lewis CJ, Coceani Paskay L, Quinzi V, Marzo G. Myofunctional therapy. Part 1: Culture, industrialisation and the shrinking human face. Eur J Paediatr Dent. 2021;22(1):80-1.
- Asiry MA. Anterior open bite treated with myofunctional therapy and palatal crib. J Contemp Dent Pract. 2015;16(3):243-7.
- Wishney M, Darendeliler MA, Dalci O. Myofunctional therapy and prefabricated functional appliances: an overview of the history and evidence. Aust Dent J. 2019;64(2):135-44.
- Fernandez-de-las-Penas C, Svensson P. Myofascial Temporomandibular Disorder. Curr Rheumatol Rev. 2016;12(1):40-54.
- Melis M, Di Giosia M, Zawawi KH. Oral myofunctional therapy for the treatment of temporomandibular disorders: A systematic review. Cranio. 2019:1-7.
Appendix O
Ten Steps for a Beautiful Smile
Books and Organizations That Are Good to Explore
- New Trends in Myofunctional Therapy, Saccmanno.Coceani Paskay
- Shut Your Mouth and Save Your Life, George Catlin (1870)
- Nutrition and Physical Degeneration, Dr. Weston Price, The
- Price-Pottinger foundation
- Cranial Osteopathy – www.cranialacademy.org
- The Brain Gym Program®, Paul & Gail Dennison
- Buteyko Breathing Technique, Patrick McKeown
- Orthotropics Facial Growth Guidance-Treatment age 2 years and up for early growth development
- International Association of Facial Growth Guidance, John & Michael Mew, DDS/William Hang, DDS
- North American Association of Facial Orthotropics (NAFFO)
- The Keys to Vocal Freedom, Suzanne Kiechle
- Tongue Tied, Richard Baxter
- AAMS, AOMT, IAOM — organizations of myofunctional therapists